Menu
About us
- 60 Years in business
- 2,000 Clients
- 50 State TPA
- 13 Years avg client relationship length
- 45-3,000 Group size
Our advantage
BeniComp IncentiCare is the only healthcare plan in the country that is able to implement an effective way to reduce spending while improving the health of your employees. Our health improvement program averages a 96% participation rate.

Because we can identify the members at risk for serious health issues, we proactively reach out to them and help them improve their health, while reducing the financial risks associated with potential health issues.

See how much you can save
What is included
Medical management
Our in-house nursing staff provides case management
Telemedicine
Members can access telehealth via video or phone call 24/7
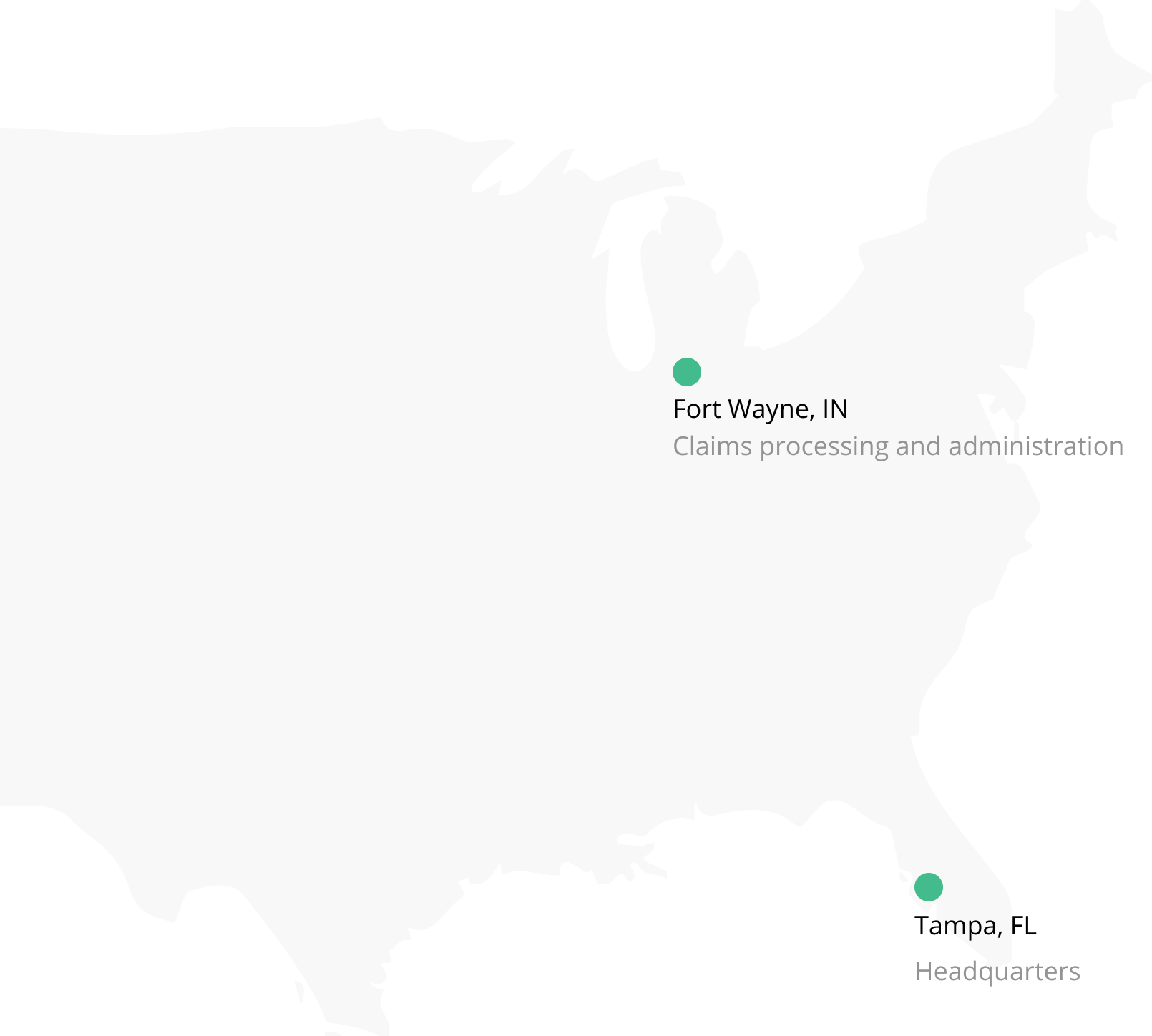
Claims processing
We provide:
- TAT statistics
- Auditing %s and ratio of accuracy
- Weekly payment of claims with invoicing and check run
Customer service
Members can connect with our support staff easily through:
- Chatting in the BeniComp Portal
- Creating support tickets
- Submitting unexpected medical bills for review
Preventive health management
In-house health coaches proactively reach out to members with poor health screening results. Access to health coaching is free for the members.
Reporting
We generate unique reports that blend data and graphics, so you can get a clear understanding of how the plan is doing.
Search
Search!

